Statistical analysis
The analyses were performed using SAS® R9.4 software (SAS Institute, Cary, NC, USA). The bilateral significance level was set at p < 0.05. All of the students’ answers, which were generally binary, were proportionally described in the general population according to the year of study. Those regarding the hyperkalemia and hypokalemia thresholds were categorized; their distribution was analyzed according to the year of study. The proportion of answers that were in keeping with the curriculum and the relevant European recommendations/literature data/expert opinions were based on indicator variables. These were created from the students’ answers, as well as the information in the curriculum and the European guidelines. Each indicator variable was rated « 1 » if the student’s answer was in keeping with the medical curriculum or the guidelines, and « 0 » if the answer was non-compliant. The results were compared according to the years of study using Fisher’s exact test, and the thresholds of dyskalemia according to the years of study were compared using a Chi2 test of homogeneity.
Results
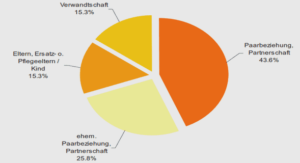
The percentage of questionnaires returned was 81.2% (n=290/357). Three questionnaires were partially completed and were not included (Figure 1).
Description of the population
The general medicine students who responded to the questionnaire were evenly distributed among the three years of internship (33.8% in the first year, 35.9% in the second year, and 30.3% in the third year).
Overall results and by the years of study and compare with the relevant guidelines
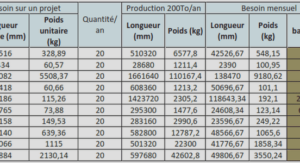
Limits of kalemia considered to be pathological
The students considered a mean hyperkalemia of 5.1 mmol/L to be pathological. The minimum hyperkalemia value proposed by one student was 3.5 mmol/L and the maximum value was 6.5 mmol/L. The mean hypokalemia considered to be pathological by the students was 3.4 mmol/L (minimum 2.5 mmol/L and maximum 3.8 mmol/L). (table 1) There was a statistically significant difference in the hyperkalemia thresholds for the different years of study (p=0.0005). Nearly a quarter of the students rated the threshold for hypokalemia as being strictly below 3.5 mmol/L (21.3%, n=61/287) (Table 1). The kalemia thresholds considered to be pathological according to the curriculum (11) and the relevant guidelines (13) were the same (hypokalemia = 3.5 mmol/L and hyperkalemia = 5.0 mmol/L). This hypokalemia threshold was indicated by 78% (n=224/287) of the students, while 60 2.1. Objectives The main objective of this study was to evaluate the knowledge of French general medicine students regarding dyskalemia. The secondary objective was to evaluate how they manage clinical situations involving dyskalemia. 2.2. Type of study All of the students (from the first to the third year of study) at the end of their general medical studies in Nancy, France, (N=357) were asked to answer a self-questionnaire, kind of like Durieu et al, regarding the perception of adverse drug reactions (10) during their final exams in June 2017. The questionnaire was in two parts: the first two questions focused on the perception of dyskalemia and the next three questions were clinical situations with open answers, to avoid influencing the answers. The questionnaire was constructed in such a way that the study reflects a general medicine context, where more information is not available at the start usually limited to the only information available in the medical report. The objective was to evaluate the student’s « reflex » management without suggesting a list of predefined answers so as not to influence the student. The answer was open-ended. The questionnaire was first tested with ten students to ensure that it was fully understood in the first round and that the answers were stable in the second round, as well as to ensure the validity of the questionnaire (11). The results were analyzed by collecting the terms in verbatim form. Thus, « monitoring under scope », « intravenous hydration », and « calcium gluconate » were classified under the term « hospitalization/emergency » as these treatments are not available in the public health care system; « taking vital signs » and « blood pressure measurement » were classified under « assessment/clinical examination ». The analysis and classification of the verbatim statements were performed after comparing the independent analyses of two authors (S. L. and B. J.M.) followed by arbitration. The answers were then compared to the treatment stipulated in the medical curriculum (from the University College of Nephrology Teachers) (12), and then to the treatment recommended by the relevant European guidelines (12,13). The answers were stratified by the years of study. 63 this hyperkalemia threshold was indicated by 66.9% (n=192/287) of the students, and 59.6% (n=171/287) of the students correctly identified both of these pathological thresholds.
Perception of danger
More than half of the general medicine students thought that severe hyperkalemia was more of a “concern” than severe hypokalemia (60.3% (n=173/287) vs. 26.5% (n=76/287)); for 10.8% (n=31/287) both types of kalemia were a concern, while for 2.4% (n=7/287) severe dyskalemia was not a concern. The students’ answers were similar across all internship years (p=0.74). There was no difference in terms of what the students had been taught regarding the danger associated with hyperkalemia versus hypokalemia. The Expert Consensus of the European Society of Cardiology has stated that hypokalemia maybe even more dangerous than hyperkalemia (14) (only 26.5% (n=76/287) of the students shared this opinion). 3.2.3. Clinical cases and comparison with evidence by medicine The students were presented with 3 hypothetical clinical situations: 1/ Isolated hypokalemia at 2.6 mmol/L (Figure 2) Most of the students stated that they would perform an electrocardiogram (ECG) (79.8%, n=229/287) and oral potassium supplementation (70.7%, n=203/287); while 16.7% (n=48/287) would provide intravenous supplementation. Half of them (53.7%, n=154/287) would request another kalemia test and 59.9% (n=172/287) would perform additional biological tests. Only a quarter of the students (28.6%, n=82/287) would undertake oral questioning and a clinical examination of the patient. They were generally not inclined to ask for advice from a specialist (28.6%, n=82/287). The further along the student was with their studies, the less likely they were to perform an electrocardiogram (ECG) in case of isolated hypokalemia (p=0.0001). On the other hand, they would more often request additional biological tests (p=0.004). The students in the second year were the most inclined to supplement with potassium (p=0.029) and they were the least inclined to refer their patients to the emergency department or to a hospital (p=0.025). There was not a statistical difference between the internship year in terms of checking the kalemia a second time (p=0.33) or performing an interview and a clinical examination (p=0.47). More than 50% of the students provided answers that were in keeping with the medical curriculum and with the data in the literature, except for the items « Interrogation/clinical 64 examination » (28.6%, n=82/287) and « Diet rich in potassium » (1.4%, n=4/287). The major difference lies in the way the patient would be supplemented with potassium: 70.7% (n=203/287) of the patients would be given an oral supplementation in accordance with the data in the literature (15,16). Indeed, interrogation, clinical examination and further investigations are essential to determine whether the patient should be hospitalized, and if so, the route of administration will be intravenous. If there is good tolerance and no signs of severity, the route of administration will be oral. There is no discrepancy between curriculum and expert opinion.