Sleep stages
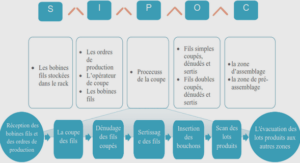
Sleep is a physiological state defined by specific characteristics (Roehrs, 2000). Being periodic, naturally-occurring, reversible, recurring and involving suspension or reduction of alertness and muscular activity, it has always been a subject of interest for researchers, even regarding the question ’why humans need to sleep?’ a scientific consensus has not been reached yet (Cirelli & Tononi, 2008). The sleep architecture is a sequence of sleep cycles, where each one is formed by different sleep stages. Each stage is characterized by specific physiological changes. There are 4 sleep stages: Rapid eye movement (REM) sleep, and three non-REM (NREM) stages: NREM1, NREM2, and NREM3 reflecting the progression from lighter (NREM1) to deep (NREM3) sleep. In 1968, Rechtschaffen and Kales (R/K) proposed the ”Manual of Standardized Terminology, Techniques, and Scoring System for Sleep Stages of Human Subjects” to score sleep stages based on pre-defined criteria of the physiological parameters measured during sleep (EA, 1969). The AASM issued the latest version to date (v.2.5.0) of the manual of sleep scoring and associated events in 2018 that is based on the R/K and researchers’ recent findings (Berry, Brooks, Gamaldo, Harding, Marcus & Vaughn, 2018). The manual is continuously upgraded. Moser, Anderer, Gruber, Parapatics, Loretz, Boeck, Kloesch, Heller, Schmidt & Danker-Hopfe (2009) compared the effects of both scoring systems on the derived scoring parameters and the overall scoring outcome. Fig. 1.1 shows a brief description of the physiological parameters changes with respect to each sleep stage, as well as the transition-specific physiological changes that are noted during transitions between sleep stages. For instance, cardiac, breathing, and body movement activities that could be measured unobtrusively are shown separately from the conventional polygraphic EEG, EOG, and EMG signals that are the gold standard used to score sleep stages, and derive the evolution of sleep stages over time, i.e., sleep hypnogram.
The burdensome impact of sleep disorders
There exist seven major categories of sleep disorders, according to the latest international classification of sleep disorders (ICSD-3) (Sateia, 2014). They can be classified as follows: 1) sleep-related breathing disorders, 2) insomnia disorders, 3) circadian rhythm sleep/wake disorders, 4) central disorders of hyper-somnolence, 5) parasomnias, 6) sleep-related movement disorders and 7) other sleep disorders. Numerous physiological dysfunctions underlaying sleep disorders have been described in the literature. Among these are neurological factors such as narcolepsy and periodic limb movement disorder (PLMD), or sleep breathing disorder (SBD) such as obstructive sleep apnea (OSA). The negative physiological impacts of sleep disorders are serious. Accordingly, studies have shown that one night of sleep deprivation can cause impairments to insulin sensitivity equivalent to a six months of a high-fat diet (Broussard & Brady, 2010). Moreover sleep disorders can alter pain tolerance in humans (Onen, Alloui, Gross, Eschallier & Dubray, 2001), can cause heart dysfunctions such us ischemic heart disease (Knutsson, Jonsson, Akerstedt & Orth- Gomer, 1986), and cause a wide range of health issues such as metabolism impairment and hormonal disturbances leading to severe physiological alterations and bad consequences (Naitoh, Kelly & Englund, 1990). Sleep disorders are not only known to induce short and long-term health issues and have bad physiological consequences (Harvey Moldofsky, 2001; Manocchia, Keller & Ware, 2001), but they are also a consequence of physiological disturbances (Misra & Malow, 2008).
In fact, occurrences of sleep disorders could also be a manifestation or a symptom displaying autonomous physiological function abnormalities that, if left untreated, could cause severe health conditions (Ribeiro, Hampton, Morgan, Deacon & Arendt, 1998). Beside health related problems, sleep disorders were shown to have a potential sociological, professional (Leger, Guilleminault, Bader, Levy & Paillard, 2002), and economical (Hillman, Murphy, Antic & Pezzullo, 2006) impact on the world population. For instance, around 150 Million people are estimated to have sleep disorders. In the United States, 50-70 million adults have a sleep disorder, 48.0% report snoring, and 37.9% reported unintentionally falling asleep during the day at least once in the preceding month (Leger, 2000; Metlaine et al., 2005; Sigurdson & Ayas, 2007). Motivated by this major prob, numerous studies were designed to make the acquisition protocol during sleep studies less obtrusive, including home-based solutions, wearable textiles, and electronic gadgets. In the next sub section, we give a brief classification of the devices types based on their relative clinical significance, and based on the world-wide established medical devices classification (Cheng, 2003).
Unobtrusively measurable physiological patterns during sleep During sleep monitoring, in order to detect abnormalities and irregularities, it is important to take into consideration the normal sleep patterns, or physiological changes that are supposed to occur during each stage. Monitoring the brain activities provides the most useful information about sleep regulation. In a PSG procedure, this is directly measured through EEG recording. The brain’s electrical activity measurements is in the range of a few hundreds of micro-volts, making it hard to measure using unobtrusive apparatus, i.e., sensors requiring a minimal contact with the subject and maintaining comfort during acquisitions. On the other hand, since the autonomic nervous system is highly influenced by the activity of the central nervous one (Shannahoff-khalsa & Yates, 2000), autonomic physiological functions such as blood pressure, muscular activity, movements, and the cardiac activity are affected and altered by the central nervous system. In addition, these autonomic functions are displayed in ample variations (millivolts for ECG, movements, or breathing) compared to the EEG’s small amplitude variations, which makes them less sensitive to noise and more suitable for unobtrusive measurement apparatus that require less stable contact with the body. Hence, unobtrusive sleep monitoring consists of capturing physiological changes such as breathing and body activity, that are alternative to conventional PSG measures such as brain and muscles activities, but without interfering with the subject’s comfort during sleep. For instance, vagal activity related features have been showing promising results that could lead to a reliable estimation of sleep hypnogram using unobtrusively acquired physiological signals. The diagram depicted in Fig. 1.3 shows three categories of sleep monitoring methods that will be addressed in this chapter: monitoring of breath disorders related parameters, monitoring of selected general sleep parameters, and unattended PSG. For each monitoring method, the physiological behavior, the acquisition method and hardware, and the obtained physiological parameters are given. In this section, each of the three activity patterns and its relationship with sleep cycles and staging is described and discussed in details.
Sleep actigraphy
Sleep actigraphy consists of recording the body’s movements during sleep. Depending on the application, the recorded data can be used to predict some insights on the neurobehavioral state, infer sleep or discern wake periods. By counting the number of body movements and assessing their amplitudes, sleep parameters, such as quality, latency, duration, efficiency, and fragmentation, circadian rhythms, sleep and wake periods, and activity levels (Gorny & Spiro, 2001). Actigraphy is convenient in sleep studies because it is a low-cost unobtrusive method that could be used in both clinics and subjects’ homes. Hence, actigraphy can be used for acquiring sleep related data in situations where PSG is logistically impractical, or for long acquisition periods in the patients home. The AASM indicates in it’s practice guidelines that actigraphy is reliable in measuring sleep for healthy adults (Morgenthaler, Alessi, Friedman, Owens, Kapur, Boehlecke, Brown, Chesson Jr, Coleman, Lee-Chiong et al., 2007). Moreover, actigraphy was shown to be sufficiently sensitive to be used in more specific applications of sleep studies. For instance, monitoring sleep changes following treatment for insomniac patients has been explored in (Brooks III, Friedman, Bliwise & Yesavage, 1993) and (Hauri & Wisbey, 1992). In 2015, the SBSM has published a guide to actigraphy monitoring, to assist clinicians and researchers using actigraphy, citing more than 150 actigraphy based works, including many on sleep applications (Ancoli-Israel, Martin, Blackwell, Buenaver, Liu, Meltzer, Sadeh, Spira & Taylor, 2015). Despite their usefulness in specific applications, sleep actigraphy systems have limitations such as inaccuracies in the number of activity accounts, and lack of clinical validation (Matar, Lina, Carrier & Kaddoum, 2018).
INTRODUCTION |