The modernization of our societies and lifestyles limits our physical movements and muscular activity. For instance, the time spent in front of a screen has drastically increased over the past years, contributing to higher daily sitting times (Owen et al. 2010). As a result, both sedentary behaviors and physical inactivity have become more common, which is not without serious health consequences: physical inactivity is indeed considered a major contributor to noncommunicable diseases, contributing to 9% of premature mortality (representing 5.3 million deaths in 2008), a burden comparable to smoking (Lee et al. 2012).
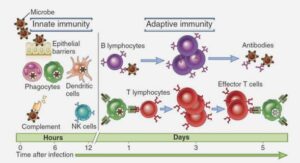
While physical inactivity is considered a risk factor for several cancer types, physical activity, on the other hand, is increasingly recognized as a strategy to limit treatment side effects, improve quality of life (QOL) and increase survival of cancer patients (Rock et al. 2012; Patel et al. 2019; Campbell et al. 2019; Friedenreich et al. 2020). Engaging in physical activity challenges whole-body homeostasis and gives rise to widespread adaptations in cells, tissues, and organ systems (Hawley et al. 2014). These pleiotropic effects have been suggested to mediate possible anti-cancer effects of physical activity, but they may also hypothetically interact with specific cancer types and/or treatments(Ashcraft et al. 2019).
Prostate cancer (PCa) is the second most diagnosed cancer in men and represents a major health issue worldwide (Bray et al. 2018). Radiotherapy (RT) is a commonly used treatment for localized PCa but its efficacy can be limited by innate or acquired radioresistance. The potential of physical activity to act as a lever to reduce these resistances remains largely unknown. The present PhD work investigates the potential for physical activity to impact tumor molecular biology and radiotherapy efficiency using different preclinical PCa models and physical activity modalities.
Prostate cancer (PCa) is a complex disease representing a major health concern around the globe, prompting the need for effective diagnostic tools and treatments. In this first chapter, we will provide an overview of the PCa epidemiology, outlining the incidence and mortality rates around the world as well as the major risk factors for this disease. Furthermore, we will describe the multistep process of prostate carcinogenesis and describe the main characteristics of malignant cells. Finally, we will summarize the currently employed diagnosis techniques and treatments used in PCa.
In 2018, an estimated 1,276,106 new cases of PCa were diagnosed around the world, representing the second most frequent malignancy in men and accounting for 7.1 % of new cancer cases worldwide (Bray et al. 2018). The PCa incidence rates vary considerably across regions, with the highest being observed in Oceania and the lowest in Asia (Bray et al. 2018; Taitt 2018). PCa is ranked as the fifth leading cause of cancer death worldwide and was responsible for an estimated 358,989 deaths in 2018 (Bray et al. 2018). The number of deaths attributed to PCa is higher in developing regions than in developed countries, which contrasts with PCa global incidence patterns (Figure L-1). As an example, 86.4 men in 100,000 were diagnosed with PCa in Australia and New Zealand in 2018, and only 10.2 in 100,000 died from this disease, while 35.9 men in 100,000 were diagnosed with PCa in Middle Africa in 2018 and 22.7 in 100,000 died from this disease (Bray et al. 2018). Considering the high incidence and relatively long survival rate of PCa, this disease unsurprisingly has a very strong prevalence. It is indeed the second most prevalent cancer behind breast cancer, with an estimated 10 million men living with PCa across the world in 2017 (IHME, 2018).
The development of PCa screening aims to decrease the mortality rates associated with this disease. Most PCa cases are diagnosed based on elevated serum levels of prostate specific antigen (PSA) (>4ng/mL) and confirmed with a tissue biopsy. The introduction of PSA testing into the population in the 1980’s has paralleled a striking increase in PCa incidence rates (Negoita et al. 2018). It also likely contributed to expanding the gap between elevated incidence rates observed in developed countries and lower rates reported in developing countries (Hassanipour-Azgomi et al. 2016), where availability and access to health care may be difficult (Quinn and Babb 2002).
PSA testing has also led to an earlier diagnosis of PCa, with an increase in the number of men diagnosed with localized disease rather than advanced stage (Thompson and Ankerst 2007; Etzioni et al. 2008). The downside of this widely used testing technique however is the increase in PCa overdiagnosis, which corresponds to cancers that may not have caused clinical consequences in the absence of screening (Loeb et al. 2014). Approximately 20 to 40% of the PCa cases in Northern America and Europe could be attributed to overdiagnosis, which questions the link between increased screening and reduced mortality (Draisma et al. 2009). Benefits from PSA testing have in fact only been recently reported: in 2018, the United States Preventive Services Task Force (USPSTF) suggested that men aged 55-69 years of age could indeed benefit from PSA testing, while it is less convincing for men over 70 years of age for whom screening may outweigh the expected harms (USPSTF 2018; Negoita et al. 2018).
Epidemiologic studies have determined several risk factors for PCa, which can be grouped into two main categories: (1) non-modifiable and (2) modifiable risk factors. Identifying these risk factors helps reducing the burden of PCa by promoting behavioral changes and by facilitating the detection of men with a higher risk of developing this disease. Importantly, PCa is a clinically heterogeneous disease with some men displaying aggressive forms of PCa while most others have a slow growing form of illness. Therefore, the risk factors for total PCa and advanced PCa may differ.
Non-modifiable risk factors, although irreversible, enable for a better understanding of the mechanisms involved in prostate carcinogenesis and help to identify individuals at high risk of developing this disease.
Aging is one of the strongest risk factors for PCa. While this disease is rare among men under 50 years of age (with an incidence of 0.1% in this population), it is estimated that 85% of PCa cases are diagnosed in men over 65 years of age (Patel and Klein 2009). This trend can be observed in both low and highly developed regions (Ferlay et al. 2015) .
Ethnicity represent another important risk factor for PCa. In the United Kingdom for example, Black men are three times more likely than White men to develop PCa (Ben-Shlomo et al. 2008) while men from South Asia have a 20% lower relative risk to develop PCa (Metcalfe et al. 2008). These observation may be explained, at least partly, by genetic factors (Kheirandish and Chinegwundoh 2011).
INTRODUCTION |