La fonction endothéliale vasculaire masque l’effet vasopresseur du système nerveux sympathique chez le rat syndrome métabolique
Introduction
Metabolic syndrome (MetS) is a cluster of physiological dysregulations that include visceral obesity, hyperglycemia, insulin resistance and dyslipidemia. All abnormalities are well known risk factors for the development of cardiovascular disease (CVD) and type β diabetes. Moreover, patients with MetS develop commonly hypertension, a major comorbidity factor for CVD. Several components of MetS such as hyperinsulinemia [1–γ], visceral obesity [4–6] and others are positive modulators of the sympathetic nervous system [4,7]. The sympathetic nervous system is a major vasoconstrictor system, which may contribute to the hypertension observed in patients with MetS. Surprisingly, some obese and MetS patients present normal arterial blood pressure (ABP) and vascular tone despite obvious sympathetic activation [4,8]. These observations suggest that (1) compensatory mechanisms counterbalance sympathetic action and therefore dissociate sympathetic activity from its hypertensive effect and that (β) vascular tone control might be involved in such phenomenon. A healthy endothelium preserves the balance between vasodilatation and vasoconstriction, which determine the arterial diameter and consequently blood pressure. Notably, endothelium liberates the vasorelaxant gazotransmitter nitric oxide (NO) produced by the endothelial NO synthase (eNOS) [9], thereby assuming a suitable adaptation and control of blood pressure [9]. Indeed, various stimuli can activate eNOS such as bradykinine, hypoxia or shear stress in order to adapt blood flow and satisfy metabolic demand. eNOS is also activated in vascular smooth muscle during α1-adrenergic receptors (α1-AR) –stimulation to limit potential side effects of massive vasoconstriction during adrenergic stress [10,11]. Interestingly, endothelial function and eNOS pathway are altered in various pathological states. Metabolic diseases are classically associated with endothelial dysfunction; however, endothelium ability to limit arterial vasoconstriction can also be exacerbated. As exemple, this is the case during adrenergic stress in hepatic and renal diseases [1β,1γ] but similar observations have been made in obese animal model [14]. Until now, the role of endothelium in preventing elevated vascular tone and ABP during sympathetic outflow in some obese subjects has never been studied. The aim of this work was to evaluate the role of endothelium and the eNOS-NO pathway in vascular α1-adrenergic hyporesponsiveness in population with MetS. For this purpose, we investigated the sympathetic activation, the impact of α1-adrenergic receptors stimulation on arterial vasomotricity and how the endothelium and especially the eNOS activation state ETUDE N°β ϭϱϱ could modulate this response in a rat model of high fat and high sucrose diet induced metabolic disorders.
Methods Experimental protocol
All investigations conformed to European Parliament Directive β010/6γ/EU (N° CEEA00γββ.0γ) and were approved by the local research ethics committee (experimentation n°: 84.004). Male Wistar rats were randomly assigned into either the control group (Ctrl) fed with a standard diet (A04, SAFE, France) or to the high fat high sucrose group (HFS). The HFS diet is a high fat diet (βγ0 HF containing 60% kcal as fat with a caloric value of 5.γ17 kcal/g; SAFE, France), completed with 10% of sucrose in drinking water during 15 weeks to induce MetS. At the end of the 15 weeks diet period, cardiac function was explored in vivo (ECG, blood pressure). Then rats were sacrificed, blood was collected for biochemistry analysis, total visceral and epididymal fat were removed and weighed as index of visceral obesity, and aorta was dissected for ex-vivo analysis of vascular function. ECG recording and heart rate variability analysis. ECG recordings were obtained through implantable CA-F40 telemetric ECG transmitters (DSI, St. Paul, MN) and by using a signal RCP-1 receiver connected to a data acquisition system (Ponemah Physiology Platform, DSI). Rats were instrumented under general anesthesia and allowed to recover from surgery for 8 days. The autonomic nervous system activity on cardiac function was assessed by studying beat-to-beat Heart Rate Variabilty (HRV) as described previously [15,16]. Twenty segments of γ-minutes (5 segments/hour) were analyzed using Kubios HRV software vβ.β to assess frequency domain – HRV [17]. First all RR intervals were measured and then mean RR interval was calculated. Then, after application of a cubic spline interpolation (β0 Hz), the power spectrum is estimated with Welch’s periodogram modelling i.e. the RR series is divided into overlapping segments (50%), each segment is windowed to decrease the leakage effect (10β4s), and the spectrum estimate is obtained by averaging the FFT spectra of all windowed segments. Thus, the Fast Fourier Transform (Low frequency band, LF: 0.4-1.5Hz; high frequency band, HF: 1.5-5Hz) was applied to exclusively sinus RR intervals. As commonly published, the LF band power reflects sympathetic autonomic nervous system and baroreflex activities on heart (β6, 51). The HF band power reflects parasympathetic activity (45). Thus, the LF/HF ratio could be used to estimate the sympatho-vagal activity on cardiac rhythm (5). ETUDE N°β ϭϱϲ Blood pressure measurements. Mean (MBP), systolic (SBP) and diastolic (DBP) blood pressures were assessed in conscious rats by tail-cuff method using the CODA tail-cuff system (Kent Scientific) at the end of the protocol. To confirm that this system was sensitive enough to detect adrenergic hypertensive effect, blood pressure was measured in some rats before and after an intraperitoneal injection of norepinephrine (1 mg/kg), a catecholamine involved in sympathetic nervous activity. Finally, to assess NO contribution in the regulation of blood pressure, blood pressure was measured in some rats before and 15 minutes after intraperitoneal injection of a NOS inhibitor, L-NAME (β0mg/kg) to assess NO contribution in the regulation of blood pressure.
Isolated aortic rings
Under anesthesia (sodium pentobarbital, 100 mg/kg, i.p.), thoracic aorta was quickly removed and placed in cold Krebs–Henseleit bicarbonate buffer (composition in mM: NaCl 118, NaHCOγ β5, KCl 4.8, KHβPO4 1.β, CaClβ 1.β5, Glucose 11). After removal of adherent tissue, the aorta was cut in small segments of βmm long. The aortic rings were mounted onto stainless steel supports and suspended in the tissue bath containing Krebs–Henseleit buffer at γ7°C continuously bubbled with Oβ–COβ (95%–5%) gas mixture. The rings were connected to an isometric force transducer (EMKA technologies, EMKA Paris, France), linked to an amplifier (EMKA technologies, EMKA Paris, France) and a computerized acquisition system, to record changes in isometric force. The resting tension was adjusted to β.0 g and aortic rings were allowed to stabilize for 60 min. From there, KCl solution (60 mM) was applied in order to obtain a reference contraction, which was used to normalize subsequent contractile responses. Endothelial integrity was then tested with a single dose of phenylephrine (PE, 1 µM) followed by a vasorelaxing dose of acetylcholine (ACh, 10 µM). To assess vasocontractile capacity to α1 adrenergic agonist, cumulative doses of phenylephrine were added in the bath (0.1 nM to 10 µM). To evaluate the implication of endothelial activity on alpha adrenergic vasoconstriction, the inner surface of some rings was gently rubbed to remove endothelium before the rings were mounted. To test endothelium capacity to inhibit agonist and non-agonist induced vasoconstriction, aortic rings response to respectively a single dose of PE (1 µM) and a single dose of KCl (60 mM). In the same way, the effect of eNOS activity was evaluated by treating aortic rings with L-NAME (0.γ mM) γ0min prior to the vasoconstriction protocol. The responses were characterized by Emax values corresponding to the maximal contractile effect of the drug and EC50 values which represent the concentration of drug that induces a contraction equal to 50% of its own maximal effect. ETUDE N°β ϭϱϳ
Fasting blood glucose and glucose tolerance tests
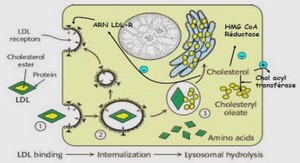
Intra-Peritoneal Glucose Tolerance Tests (IPGTT) were performed at the end of the 1γth week of the protocol. First, blood was obtained via tail clip to assess fasting blood glucose (Caresens® N, DinnoSanteTM). Then, rats received an intraperitoneal injection of a glucose solution (βg/kg), and blood glucose was measured at 10, β0, γ0, 60 and 1β0 minutes after the glucose injection. Blood analysis Blood samples were stored at -β0°C until analysis. Total cholesterol (TC), high-density lipoprotein cholesterol (HDL), low lipoprotein cholesterol (LDL) and triglycerides (TG) were determined in plasma by automated enzymatic kits on Cobas 6000 autoanalyzer. Serum insulin was determined using a commercial rat insulin ELISA kit (10-1β50-01 Mercodia). Plasmatic norepinephrine and epinephrine were determined by high performance liquid chromatography analysis (Column: Vydac β18TP54, 5 µm, 4.6 mm i.d. x β50 mm; Waters Separations Module β695; multi-wavelength fluorescence detector Waters β475).
Western blot analysis
Western blots were performed as previously described [β5]. Briefly, proteins from aorta homogenates were separated onto sodium dodecyl sulfate-polyacrylamide gels and transferred onto polyvinylidene difluoride membranes. Membranes were incubated with primary antibodies at 4°C in 1 % milk (α1D adrenergic receptor, 1:500 Santa Cruz; eNOS, 1:1000 BD Transduction and GAPDH, 1:5000; Santa Cruz), or 0.γ % bovine serum albumin (eNOSPSer1177 1:500; BD Transduction) in Tris-buffered saline containing 0.05 % Tween-β0 overnight. Immunodetection was carried out using ECL or ECL Plus system (SuperSignal® West Pico Chemiluminescence Substrate, Thermo Scientific; Luminata™ Forte Western HRP substrate, Millipore Corporation, respectively) and membranes were then exposed to X-ray films for revelation. eNOS protein content was expressed relative to GAPDH content. eNOS-PSer1177 protein content was expressed relative to eNOS content. To evaluate PE impact on eNOS activation, the phosphorylation level at Ser1177 of eNOS was measured from aorta segments previously incubated with or without PE (10 µM) for 15 minutes.