Formation comparaison de deux systèmes d’aphérèse des lipoprotéines, tutoriel & guide de travaux pratiques en pdf.
Methods
Population
Nine HoFH subjects were recruited from a pool of patients being followed at the lipid clinic of the Laval University Medical Center in Quebec City. All participants were at least 15 years old. None of the subjects were pregnant or nursing; had acute liver disease, hepatic dysfunction, or persistent elevations of serum transaminases; had a recent history of alcohol or drug abuse; had diabetes mellitus; had a history of cancer; or had undergone hormonal treatment. They were all taking lipid lowering medications and were receiving LA bimonthly.
All patients were screened for mutations in the LDLR gene from samples of their genomic DNA; the deletion mutations were detected by Southern blotting,15 and the point mutations were analyzed by restriction enzyme fragment analysis.3,16 Four patients were found to be compound heterozygous, carrying a >15 kb deletion at the 5’ end of the gene5 and the W66G mutation in exon 3,17 two were homozygotes for the >15 kb deletion at the 5’ end of the gene,5 two were homozygotes for the W66G mutation in the exon 3,17 and one subject, from Honduras, had a splice site mutation in intron 7 (LDL-R1061(-1) G–>C).18
Study Design
Subjects were first treated with the HELP system then with DS in this single sequence study. The mean time interval between each apheresis was 34 days (median: 28 days).
Fasting blood samples were obtained at the beginning and at the end of each LA. For DS, two subjects had their blood samples taken before and after two separate lipid apheresis treatments: one stopped after 3,000 mL of plasma filtration (DS3) and the other stopped after completion of the treatment (DSF>4 L). All other patients (n = 7) had their DS3 and DSF blood samples taken during a single treatment.
The study was approved by the Laval University Medical Center ethical review committee, and written informed consent was obtained from each subject. This trial was registered at clinicaltrials.gov as NCT02286596.
Heparin-induced Extracorporeal LDL Precipitation
HELP LA was performed using the Plasmat Futura® system (B. Braun Medical, Bethlehem, PA, USA). It has been proven useful in decreasing total cholesterol, LDL-C, lipoprotein (a) Lp(a) and C-reactive protein (CRP). According to manufacturer’s specifications, the maximum volume of plasma filtrated using the Plasmat Futura® is 3 L. After primary separation from other blood constituents, the plasma is mixed with an acetate-acetic acid buffer (pH 4.85), so that the pH of the mixture is 5.1. Then, 100,000 U heparin per liter is added to the buffer. After the plasma has been mixed thoroughly with the acetate-acetic acid buffer and heparin, LDL-C precipitates in the acid environment together with fibrinogen and heparin. These precipitates are then removed from the plasma by a polycarbonate membrane. The remaining free heparin is almost completely removed by a heparin absorber (DEAE cellulose). The acidemic plasma is returned to a physiological pH value using bicarbonate dialysis, and the plasma, free of LDL, is returned to the patient with the blood cells.
Dextran sulfate adsorption
LA with DS was performed using the Liposorber® LA-15 system (Kaneka Corporation, Osaka, Japan). The manufacturer’s specifications recommend treating 1.5 patient plasma volumes during a single procedure to yield a 75 to 80% acute reduction in plasma LDL-C concentrations. The plasma volume for each patient was estimated using the following equation: plasma volume (L) = 0.065 X weight (kg) X (1-hematocrit).19 After primary separation, the plasma is pumped into one of the two dextran sulfate adsorption columns. ApoB-containing lipoproteins electrostatically bind in the first column to the negatively charged dextran sulfate. The plasma is then transferred to the other column, and the first column is rinsed with NaCl to remove LDL-C. Both columns work in alternating cycles. The plasma is then mixed with blood and passes through a warmer column before being reinjected into the patient. Heparin is used as an anticoagulant during the treatment.9,20
Plasma lipids, Lipoproteins and Apoproteins
Blood samples were collected in tubes containing disodium EDTA (Na2EDTA) and benzamidine (0.03%).21 Samples were immediately centrifuged at 4°C for 10 min at 3,000 rpm to obtain plasma and were stored at 4°C until processing. The cholesterol and triglyceride (TG) levels were determined in the plasma and lipoprotein fractions by enzymatic methods (Randox Co., Crumlin, UK) using an Olympus AU400 analyzer (Melville, NY, USA), as previously described.22 Plasma VLDL (d < 1.006/mL) were isolated by preparative ultracentrifugation, and the HDL fraction was obtained after precipitation of LDL in the infranatant (d > 1.006 g/mL) using heparin and MnCl. The cholesterol and TG contents of the infranatant fraction were measured before and after the precipitation step. Plasma apoB and apoA-I levels were measured using a BN-ProSpec nephelometer (Dade Behring, Mississauga, Ontario, Canada) with reagents and calibrators provided by the manufacturer.
Plasma PCSK9, Lipoprotein (a), Inflammatory Markers, and Adhesion Molecules
Commercial enzyme-linked immunosorbent assay (ELISA) kits were used to measure plasma PCSK9 (Circulex, CycLex Co, Nagano, Japan), lipoprotein (Lp) (a) (ALPCO, Salem, NH, USA), C-reactive protein (CRP) (BioCheck, Inc. Foster City, CA, USA), plasma interleukin-6 (IL-6), tumor necrosis factor- (TNF-), vascular cellular adhesion molecule-1 (VCAM-1), intercellular adhesion molecule-1 (ICAM-1) and E-selectin (R&D Systems, Minneapolis, MN, USA) following the manufacturer’s instructions.
LDL Particle Size Measurement
Various measures of LDL particle size, including the LDL peak particle diameter (LDL-PPD) and the proportion of small and large LDL, were assessed using nondenaturing 2%-16% polyacrylamide gel electrophoresis as described previously.23
Statistical analysis
The PROC MIXED procedure was used to compare pre-post values and the differences between each apheresis treatment. The covariance structure was adjusted for each variable to increase the power of the test. Non-normally distributed variables were transformed prior to the analyses. The Boxcox procedure was used to determine the adequate transformation to normalize the variables. The Tukey-Kramer adjustment was used to account for the repeated measures. Differences were considered significant at P ≤ 0.05. All analyses were performed using SAS (v9.3, SAS Institute, Cary, NC).
Results
Subjects
The demographic, anthropometric and genotypic characteristics of the subjects (4 men and 5 women) are presented in Table 1. The median age was 44 years (range: 15-53 years), the median weight was 75.7 kg (51.0-121.5 kg) and the median body mass index was 24.7 kg/m2 (19.9-37.5 kg/m2). As mentioned earlier, two subjects were homozygotes for the >15 kb deletion, two were homozygotes for the W66G mutation, four were compound heterozygotes carrying the >15 kb deletion and the W66G mutation, and one subject was homozygote for a splice site mutation in intron 7 (LDLR1061(-1) G–>C mutation).
Technical Aspects
Using the Plasmat Futura® system (HELP), 3000 mL of plasma was filtered during the treatment. The Liposorber® system (DSF) allowed for a larger plasma volume to be filtered, with a median volume of 4200 mL (3100-4500; P=0.0002). Compared with DS, the plasma filtration rate was higher with the HELP system (24.0 mL/min (16.7-31.6 mL/min) vs. 18.7 mL/min (12.9-23.3 mL/min); P=0.006).
Lipids/Lipoproteins
Table 2 presents pre-post values for plasma lipids, PCSK9, Lp(a), LDL size, and LDL-PPD following LA treatments. LA with both HELP and DSF significantly decreased total cholesterol, TG, total apoB, VLDL-C, LDL-C, HDL-C, PCSK9, and Lp(a). Except for Lp(a), significant reductions in these parameters were also achieved after 3000 mL of plasma filtration with the DS system (DS3). LA with HELP had no impact on either LDL size or LDL-PPD. LDL size was not affected by treatment with DS3 but was reduced when a larger plasma volume was filtered using DSF (P=0.08). LDL-PPD was significantly reduced following DSF.
The median reductions in the plasma lipids, PCSK9, and Lp(a) levels following each LA are compared in Table 3. For the same filtered plasma volume, apheresis with HELP led to a greater reduction in the plasma apoB, HDL-C and PCSK9 levels. Changes in total cholesterol, plasma TG, and LDL-C were not significantly different between apheresis treatments with the same volume of plasma filtration (HELP vs. DS3).
Compared with HELP, apheresis with DSF led to significantly greater reductions in total cholesterol, VLDL-C, and LDL-C. In addition, the reduction in HDL-C was smaller after DSF compared with HELP. Finally, the decrease in the PCSK9 and Lp(a) levels were not significantly different between apheresis treatments with HELP and DSF.
Compared with DS3, filtration of a larger plasma volume using the DSF protocol led to significantly greater reduction in total cholesterol, apoB, and LDL-C. However, there were no significant changes in TG, VLDL-C, HDL-C, PCSK9, and Lp(a) between DSF and DS3.
Adhesive Molecules and Inflammatory Markers
The pre-post treatment values for ICAM-1, VCAM-1, E-selectin, CRP, TNF-α, and IL-6 for each LA system are presented in Table 4. No significant changes in the ICAM-1 and VCAM-1 levels were observed after apheresis with the HELP or DS system. The E-selectin and CRP levels, however, were significantly reduced following apheresis with HELP, DS3 and DSF (E-selectin: P≤0.02, and CRP: P≤0.001,). The TNF-α levels were significantly decreased after treatment using DS3 and DSF. In contrast, LA treatment with HELP, DS3 and DSF significantly increased IL-6 levels.
As shown in Figure 1A, reduction in the E-selectin levels was not significant between HELP, DS3 and DSF. Figure 1B shows that the greatest reduction in CRP was achieved with DSF (P<0.01). Reduction in the TNF-α levels was similar using DS3 and DSF (P=0.80), whereas HELP had no effect on TNF-α levels (Figure 1C). Finally, changes in the IL-6 levels were significantly greater after treatment with DS3 and DSF compared with HELP (P<0.001) (Figure 1D).
Discussion
This is the first study to compare the efficacy of LA treatment using HELP or DS in the same HoFH subjects. Our results demonstrate that LA treatment using HELP or DS is effective to reduce plasma lipid levels and several inflammatory markers and adhesion molecules. Compared with HELP, DSF led to significantly greater reductions in the total cholesterol, VLDL-C, LDL-C, and HDL-C levels. For the same volume of filtered plasma (3000 mL), however, HELP led to a greater reduction in apoB, VLDL-C, HDL-C and PCSK9 levels. Moreover, both systems significantly reduced CRP and E-selectin levels, but only DS significantly lowered TNF-α concentrations. In contrast, IL-6 was significantly increased following treatment with both systems.
LA is used as a long-term therapy to rapidly reduce plasma lipids and lipoproteins in patients with homozygous or severe heterozygous FH who are intolerant or not sufficiently responsive to lipid-lowering therapy. As expected, both LA techniques (HELP and DS) were highly effective in reducing the concentrations of apoB-containing lipoproteins and cholesterol in subjects with HoFH. Marked reductions in the concentrations of atherogenic lipoproteins with LA have been shown to reduce the rate of cardiovascular events in FH patients.24 Sachais et al.25 reported that treatment with LA over a 7-year period in patients with severe hypercholesterolemia was associated with a significant decrease in cardiovascular events and interventions. This study showed a 3.7-fold reduction in the relative risk for cardiovascular events and an over 20-fold decrease in the relative risk for cardiac interventions.
In this study, HELP led to a greater reduction in the HDL-C levels than LA with DS. Both devices (HELP and DS) remove LDL and other lipoproteins through interactions between polyanions and apoproteins. The negatively charged DS filter and the low pH acetate buffer with polyanion heparin (HELP) have been shown to form insoluble precipitates with the positively charged amino acid domains of apoB. In contrast, HDL is negatively charged and does not contain apoB. This difference in the structure and charge of HDL most likely accounts for the fact that changes in the plasma HDL content are less dramatic than those observed for apoB-containing lipoproteins. Previous studies reported that LA treatment achieved a slight decrease in HDL-C levels,26,27 a finding attributed to hemodilution, activation of hepatic triglyceride lipase, or decreased activity of lecithin cholesterol acyltransferase.28 Our results, however, suggest that DS may decrease HDL-C significantly less than HELP. Further studies are needed to investigate the mechanisms underlying the differences in HDL-C responses following LA using either HELP or DS.
In this study, LA performed with the HELP technique did not affect the mean LDL size and LDL PPD. The LDL pool before and after HELP apheresis was mainly composed of medium size LDL particles (255-265 Å). However, treatment with the DS technique was associated with a significant decrease in LDL PPD and a tendency to reduce LDL particle size. Small, dense LDL (sdLDL) particles (<255 Å) have been shown to be more atherogenic, and an increase in the relative proportion of sdLDL has been correlated with higher CVD risk.29,30 These results are in contrast with a previous finding by Schamberger et al.31 who reported a significant reduction in sdLDL particles and a significant increase in large LDL particles following apheresis treatment with both HELP and DS techniques in 16 FH subjects. It is important to emphasize that the variations in LDL particle size and LDL PPD following LA are expected to be much less predictive of future CV events than variations in the levels of apoB-containing lipoproteins. Further studies are required to clarify the impact of LA on the LDL density profile.
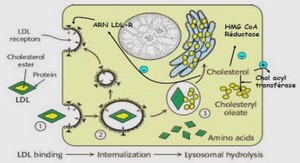
Our results are in agreement with previous findings10 showing that LA reduces plasma PCSK9 levels. PCSK9 is the ninth member of the proprotein convertase family and is mainly expressed in the liver, small intestine and kidney.32 Mechanistic studies have shown that PCSK9 interacts with the epidermal growth factor precursor homology domain A of the LDLR at the cell surface and promotes its intracellular lysosomal degradation.33 High levels of PCSK9 decrease the LDLR density on the cell surface and, therefore, reduce LDL-C clearance, leading to an accumulation of LDL particles in plasma.34 PCSK9 has an impact on apoB and Lp(a) synthesis by inhibiting the degradation of newly synthesized apoB.35 LDL-C levels and PCSK9 levels have been shown to be positively correlated in non-FH and untreated FH subjects,36,37 with PCSK9 levels being higher in HoFH than in heterozygous FH or non-FH patients.38 Our results show that LA with HELP led to a greater reduction in the PCSK9 levels than LA using DS3. We did not observe, however, a significant correlation between changes in LDL-C and changes in PCSK9 levels. Therefore, reduction of the PCSK9 levels is an additional benefit of LA in HoFH. One can speculate that LDL-C levels would more rapidly return to baseline without a drop in PCSK9 levels, which could be responsible for the maintenance of low LDL-C levels after each apheresis treatment.
Lp(a) is an important independent CVD risk factor.39 Maintaining low levels of Lp(a) is important in the treatment of HoFH. In our study, the decrease in Lp(a) levels was similar with various LA protocols, achieving a reduction of 65.0% with HELP, 65.4% with DS3 and 70.6% with DSF. These results suggest that both LA systems are effective for reducing Lp(a) levels in HoFH.