Secondary Cataract
Introduction
Secondary cataract or posterior capsule opacification (PCO) is the most common post-operative complication of cataract surgery. Its incidence has decreased over the past few decades as the understanding of its pathogenesis has evolved. Advances in surgical technique, intraocular lens (IOL) design and materials have all contributed to the gradual decline in PCO incidence. However it remains a major cause of decreased visual acuity after cataract surgery, occurring at a rate of between 3–50% in the first five post-operative years.
PATHOGENESIS
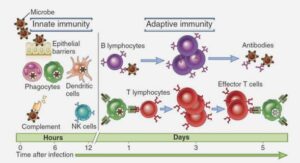
PCO results from migration and proliferation of residual lens epithelial cells (LECs) onto the central posterior capsule. When the cells invade the visual axis as pearls, fibrotic plaques, or wrinkles, the patient experiences a decrease in visual function, and ultimately in visual acuity.2 The epithelium of the crystalline lens consists of a sheet of anterior epithelial cells (‘A’ cells) that are in continuity with the cells of the equatorial lens bow (‘E’ cells). The latter cells comprise the germinal cells that undergo mitosis as they peel off from the equator. They constantly form new lens fibers during normal lens growth. Although both the anterior and equatorial LECs stem from a continuous cell line and remain in continuity, it is useful to divide these into two functional groups. They differ in terms of function, growth patterns, and pathologic processes. The anterior or ‘A’ cells, when disturbed, tend to remain in place and not migrate. They are prone to a transformation into fibrous-like tissue (pseudo-fibrous metaplasia). In contrast, in pathologic states, the ‘E’ cells of the equatorial lens bow tend to migrate posteriorly along the posterior capsule; e.g., in posterior subcapsular cataracts, and the pearl form of PCO. In general, instead of undergoing a fibrotic transformation, they tend to form large, balloon-like bladder cells (the cells of Wedl). These are the cells that are clinically visible as ‘pearls’ (Elschnig pearls). These equatorial cells are the primary source of classic secondary cataract, especially the pearl form of PCO. In a clinical study by Neumayer and coworkers, significant changes in the morphology of Elschnig pearls were observed within time intervals of only 24 hours. Appearance and disappearance of pearls, as well as progression and regression of pearls within these short intervals illustrate the dynamic behavior of regeneratory PCO.3 The ‘E’ cells are also those responsible for formation of a Soemmerring’s ring, which is a doughnut-shaped lesion composed of retained/regenerated cortex and cells that may form following any type of disruption of the anterior lens capsule. This lesion was initially described in connection with ocular trauma. The basic pathogenic factor of the Soemmerring’s ring is the anterior capsular break, which may then allow exit of central nuclear and cortical material out of the lens, with subsequent Elschnig pearl formation. A Soemmerring’s ring forms every time any form of extracapsular cataract extraction (ECCE) is done, whether manually, automated, or with phacoemulsification (phaco). For practical purposes it is useful to consider this lesion as the basic precursor of classic PCO, especially the ‘pearl’ form. The LECs have higher proliferative capacity in the young compared with the old, therefore, the incidence of PCO formation is higher in younger patients. The same cell types mentioned above are also involved in other processes of opacification within the capsular bag (Fig. 5-16-1). These include anterior capsule opacification (ACO),4,5 and interlenticular opacification (ILO).6,7 This latter is the opacification of the space between two or more IOLs implanted in the bag (piggyback implantation).
Treatment and Prevention
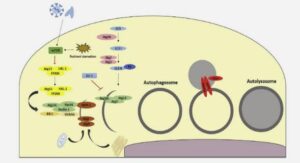
The treatment of PCO is typically neodymium : YAG (Nd : YAG) laser posterior capsulectomy. This is a simple procedure in most cases, but is not without risks. Complications include IOL damage, IOL subluxation or dislocation, retinal detachment, and secondary glaucoma.8 Therefore, prevention of this complication is important, not only because of the risks associated with its treatment, but also because of the costs involved in the procedure. Extensive research has been performed on the inhibition of LEC proliferation and migration by pharmacologic agents through various delivery systems, or IOL coatings, in vitro and in vivo animal studies.9–11 Use of pharmacological and nonpharmacological agents for this purpose in an unsealed system may increase the risk of toxicity to surrounding intraocular structures, especially corneal endothelial cells. The PerfectCapsule™, a silicone device that reseals the capsular bag allowing isolated safe delivery of irrigating solutions into its inner compartment, was therefore developed.12 Immunotherapy and gene therapy, as well as physical techniques to kill/remove LECs have also been investigated.13,14 We have evaluated in our laboratory the efficacy of a Nd : YAG laser photolysis system in removing LECs using human cadaver eyes. Light microscopy and immunohistochemistry revealed that the laser photolysis system removed LECs from the anterior lens capsule and capsule fornix. Along with the cells, laminin, fibronectin, and cell debris remained in the untreated areas but were removed by the treatment, which may be useful for PCO prevention.14 While basic research on an effective mechanism for PCO eradication evolves, the practical surgeon can already apply some principles to prevent it.15 Studies done in our laboratory, as well as clinical studies done in other centers, have helped in the definition of three surgery-related factors that help in the prevention of PCO: Hydrodissection-enhanced cortical clean-up, In-the-bag IOL fixation, and Performance of a capsulorrhexis slightly smaller than the diameter of the IOL optic (Fig. 5-16-2). The same studies helped in the definition of three IOL-related factors for PCO prevention: Use of a biocompatible IOL to reduce stimulation of cellular proliferation, Enhancement of the contact between the IOL optic and the posterior capsule, and An IOL with a square, truncated optic edge.