Materials and Methods
Patients
Ten HoFH patients and five compound heterozygous patients with genetically defined LDLR mutations were included in this study. The HoFH patients were carriers of the W66G mutation in exon 3 (n=3),13 the >15-kb deletion at the 5’ end of the gene (n=5),14 the splice site mutation in intron 7 (LDLR1061(-1) G to C) (n=1)15 and the C660X Lebanese alleles (n=1).16 Four compound heterozygous subjects were carriers of the W66G mutation and the >15-kb deletion and one subject was a carrier of the C646Y mutation in exon 1417 and the >15-kb deletion. The >15-kb deletion at the 5’ end of the gene, the splice site mutation in intron 7, the C646Y mutation in exon 14 and the C660X mutation were considered receptor-negative mutations. The W66G point mutation in exon 3 was categorized as a receptor-defective mutation. All subjects were treated with maximally tolerated doses of statin and ezetimibe during the duration of the study.
Study design
Data from consecutive LA treatments (n=2124) performed between August 2008 and February 2016 at the CHU de Québec-Laval University were collected. For each patient, the compiled data included, when available: 1) the date of LA, 2) the cumulative number of LA treatments received, 3) the interval (in days) between LA treatments, 4) the type of LA system used, 5) the volume of plasma that was filtered per treatment, 6) the duration (in minutes) of the treatments, 7) the pre- and post-LA serum lipid concentrations and 8) the cumulative interval since the first LA treatment (in days). The LA-induced acute decrease in serum lipids was calculated as the percent difference between the post-LA and pre-LA serum lipid concentrations. This study was approved by the Laval University Medical Center ethical review committee and informed consent was obtained from each patient.
La systems
The HELP and the DSA LA systems were used in this study. HELP LA was performed using the Plasmat Futura® system (B. Braun Medical, Bethlehem, PA, USA). The maximum volume of plasma that could be filtered using this system was 3000 mL, until late 2015 when new filters that increased the maximum volume of plasma that could be filtered to 4000 mL were made available in Canada. LA by DSA was performed using the Liposorber® LA-15 system (Kaneka Corporation, Osaka, Japan). This system has been used at the Lipid Clinic of the CHU de Québec-Laval University since 2012. The technical procedures for the HELP and DSA systems have been previously described.11 All subjects experienced the two LA systems during the study period.
Determination of serum lipid concentrations
For routine LA therapy, patients are not instructed to fast before treatments. Blood samples were obtained pre- and post-LA. Serum cholesterol and TG concentrations were determined with a Roche/Hitachi MODULAR analyzer (Roche Diagnostics, Indianapolis, IN, USA) using the appropriate reagents. The LDL-C concentration was calculated using the Friedewald equation.18 In 24 out of 2124 treatments (1.1% of the total compiled treatments), the LDL-C concentration was not calculated because the TG concentration was > 4.50 mmol/L. Lp(a) concentrations were measured by nephelometry using a BN ProSpec system (Siemens Healthcare, Erlangen, Germany).
Statistical analyses
Statistical analyses were conducted with the JMP Pro software v12.2.0 using mixed models for repeated measures. In the models, the acute LA-induced reduction in lipid concentrations was the dependent variable. Pre-LA TG concentrations and other potential covariates were included in the models as independent variables and were treated as fixed effects. Subjects were treated as a random effect. The patient-specific time interval since the first compiled LA for each treatment was treated as the repeated measure in the models. The spatial power covariance structure was used for all the models because the time intervals between treatments were unequally spaced. The models only included treatments without missing covariates and with TG concentrations < 4.50 mmol/L, i.e. models with the acute LA-induced reduction in LDL-C as a dependent variable included n=1761 treatments and models with the LA-induced acute decrease in Lp(a) as a dependent variable included n=1391 treatments. The normality of the models was assessed using the distribution of the scaled residual values. The Tukey-Kramer adjustment was used for multiple comparison tests. Statistical significance was set to p <.05.
Results
The mean age of the patients in this study was 34.2 ± 14.3 years (Table 1). They were treated with maximally-tolerated doses of statins (atorvastatin: 80 mg, n=7; 40 mg, n=1; rosuvastatin: 40 mg, n=6; 5 mg, n=1) and ezetimibe (10 mg; n=14). Eight subjects had a history of CAD at baseline. Patients exhibited typical characteristics of HoFH, elevated concentrations of total-C, LDL-C and Lp(a). Prior to the first compiled LA, patients with receptor-negative HoFH exhibited higher total-C and LDL-C concentrations than patients with receptor-defective HoFH. Although carriers of the receptor-negative mutations exhibited approximately 2-fold higher average TG concentrations than carriers of the double receptor-defective mutations, the difference was not significant (p=.2). There was no difference in the Lp(a) concentrations between the LDLR genotypic groups (p=.5). There was considerable intra-genotype variability in Lp(a) concentrations (defective/defective, range: 374-692 mg/L; defective/negative, range: 419-1,140 mg/L; negative/negative, range: 121-1,500 mg/L).
As presented in Table 2, the use of the two systems between the LDLR genotypes was unequal (p <.0001). Patients with double receptor-negative mutations were treated more often with the DSA system than patients with receptor-defective mutations. The average volume of filtered plasma per treatment was significantly higher in patients with double receptor-negative mutations, likely due to the more frequent use of the DSA system.
A significant association between pre-LA TG concentrations and the acute LA-induced reduction in LDL-C, modified by the type of LA system, was observed (p pre-LA TG quartile * LA system=.04). The acute reduction in LDL-C using the DSA system was 3.9% lower when pre-LA TG concentrations were >2.09 mmol/L (highest quartile) than when pre-LA TG concentrations were ≤0.93 mmol/L (lowest quartile) (-59.4 ± 3.1% vs. -63.3 ± 3.0%, p=.007) (Figure 1). However, pre-LA TG concentrations had no effect on the reduction in LDL-C when the HELP system was used (p inter-quartiles ≥.7). The interaction between the type of LA system used and the pre-LA TG concentrations on the LA-induced acute reduction in LDL-C was independent of the LDLR genotype, type of lipid-lowering medication, cumulative number of LA treatments, volume of plasma that was filtered, LA treatment frequency, cumulative interval since the first compiled LA and the pre-LA LDL-C concentrations. Similar results were obtained when the analysis was conducted on the absolute reduction in concentrations of LDL-C (mmol/L).
Significant associations between pre-LA TG concentrations and the acute LA-induced reduction in non-HDL-C and in total-C, modified by the type of LA system, were observed (non-HDL-C: p pre-LA TG quartile * LA system=.03; total-C: p pre-LA TG quartile * LA system=.04). The acute reduction in non-HDL-C and total-C using the DSA system was reduced by respectively 3.8% (p=.008) and 3.7% (p=.004) when pre-LA TG concentrations were >2.09 mmol/L (highest quartile) compared with pre-LA TG concentrations ≤0.93 mmol/L (lowest quartile) (Figure 2A and B). Pre-LA TG concentrations were not associated with the LA-induced acute reduction in non-HDL-C and total-C when the HELP system was used (p inter-quartiles ≥.9).
The LA-induced acute reduction in HDL-C was significantly more important using the HELP system (p <.0001), independent of pre-LA TG levels. The acute reduction in HDL-C was lower when pre-LA TG concentrations were >2.09 mmol/L (highest quartile) than when pre-LA TG concentrations were ≤0.93 mmol/L (lowest quartile) using both the DSA system (-7.1 ± 2.3% vs. -10.1 ± 2.4%, p=.002) and the HELP system (-18.5 ± 2.1% vs. -20.8 ± 2.1%, p=.002) (Figure 2C).
Pre-LA TG concentrations were inversely associated with the acute LA-induced reduction in TG. The acute reduction in TG was lower when pre-LA TG concentrations were >2.09 mmol/L (highest quartile) compared with pre-LA TG concentrations ≤0.93 mmol/L (lowest quartile) using both the DSA system (-55.6 ± 6.6% vs. -25.3 ± 6.8%, p <.0001) and the HELP system (-47.2 ± 6.0% vs. -38.4 ± 5.9%, p=.0009) (Figure 2D).
Supplemental Table 1 presents the comprehensive, non-adjusted, absolute, pre-LA, post-LA and LA-induced reduction in lipid concentrations.
No association was observed between the pre-LA TG concentrations and the LA-induced acute decrease in Lp(a) (p=.2). The systems also had no differential effect on the reduction of Lp(a) concentration (p pre-LA TG * LA system=.7). The observations were similar when the analysis was conducted on the absolute reduction in Lp(a) concentration (mg/L).
Compared with LA by HELP, LA by DSA induced a relatively less important decrease in LDL-C (Δ=-4.7 ± 0.6%, p <.0001) and Lp(a) (Δ=-4.6 ± 1.0%, p <.0001) levels over the duration of the study after adjusting for pre-LA TG levels and the volume of plasma that was filtered. However, without the adjustment for the filtered plasma volume, LA by DSA was more effective than LA by HELP in reducing serum concentrations of LDL-C (Δ=+8.9 ± 0.6%, p <.0001) and Lp(a) (Δ=+5.1 ± 0.9%, p <.0001). The average volume of filtered plasma per treatment was significantly higher with DSA than with HELP (4,147 ± 706 vs. 2,961 ± 204 mL, p <.0001).
Discussion
This retrospective longitudinal study evaluated how pre-LA TG concentrations modified the efficacy of two different LA systems to acutely reduce the concentrations of LDL-C and Lp(a) in patients with HoFH. Our observations demonstrate that elevated pre-LA serum TG concentrations attenuated the acute decrease in LDL-C when using the DSA system, but not when using the HELP system. These observations were independent of various factors associated with LA efficacy, namely, pre-LA LDL-C or Lp(a) concentrations, the volume of filtered plasma, the LDLR genotype, and the interval between consecutive treatments. Our data suggest that LA therapy should be adapted according to pre-LA TG concentrations to maximize its efficacy among patients with HoFH.
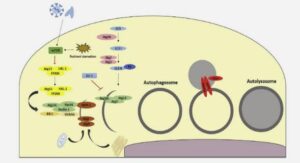
In the DSA system, after primary separation, the plasma is pumped into one of two DSA columns. ApoB-containing lipoproteins electrostatically bind to the negatively charged dextran sulfate cellulose beads. The plasma is then transferred to the other column and the first column is rinsed to remove the apoB-containing lipoproteins. Both columns work in rotation during treatment. It is estimated that 2.5 grams of lipoproteins can be adsorbed by each column every cycle.19 The plasma is then mixed with blood, passes through a warmer column, and is re-injected into the patient’s venous circulation. Heparin is used as an anticoagulant during the treatment.10 In the HELP system, after primary separation from the other constituents of the blood, the plasma is mixed with heparin and an acetate-acetic acid buffer to reduce the pH of the mixture to approximately 5. At this pH, apoB-containing particles are negatively charged and heparin is positively charged.10 After the plasma has been mixed thoroughly with the acetate-acetic acid buffer and heparin, LDL-heparin complexes are formed and precipitate in the acidic environment. These precipitates are removed from the plasma by polycarbonate membrane filtration. Finally, the remaining free heparin is removed by adsorption, the acidic plasma is returned to a physiological pH value, and the LDL-depleted plasma is returned to the patient’s venous circulation.10
Based on our observations, the interaction between apoB-containing lipoproteins and dextran sulfate is reduced when the total serum TG concentrations are high, when the TG-content of apoB-containing particles is elevated or when the LDL particles are small and dense.20 The electrostatic affinity between apoB-particles and dextran sulfate is likely impaired in TG-rich plasma. It is also possible that the adsorption of large TG-rich apoB-containing particles reduces the residual available contact surface between the apoB particles and dextran-sulfate. Finally, small cholesterol-rich LDL particles, highly prevalent in the plasma of HoFH patients with high TG levels,20 may have a reduced affinity for dextran sulfate compared with larger particles. Moreover, since pre-LA TG concentrations were not associated with an acute LA-induced reduction in Lp(a) levels, the presence of apo(a) on LDL particles compared with LDL alone may enhance the interaction between the adsorbate and the adsorbent. The efficacy of the HELP system to acutely reduce LDL-C and Lp(a) levels was not impaired by pre-LA TG concentrations. Based on the technical procedures of this system, we hypothesized that, independent of plasma TG concentrations, lipoprotein TG-content or LDL size, the mixing step prior to precipitation allows for a large contact surface area between apoB-containing particles and heparin. Extensive studies are required to characterize the exact mechanism underlying the observed effects.
We observed that the LA-induced acute reduction in HDL-C levels was more important with the HELP system than with the DSA system. Elevated plasma levels of apoE-rich HDL particles is a phenotypic characteristic of FH.21 Moriarty et al22 previously observed that LDL apheresis using HELP and DSA acutely reduces the plasma levels of apoE. The reduction in apoE was associated with the pre vs. post change in HDL-C. Although HDL is a negatively charged particle, apoE is positively charged and interacts with heparin and dextran sulfate.22 ApoE is suspected to be responsible of the LA-induced acute reduction in HDL-C. Investigation is required to identify mechanisms underlying the differential effect of LA with HELP and DSA on HDL-C removal.
Despite the reduced efficacy associated with elevated TG levels, LA by DSA remained more effective than LA by HELP for the acute removal of LDL-C from plasma because of its higher filtration capacity (>4000 mL vs. ≤4000 mL), independent of TG concentrations, as previously observed.11 In an era of precision medicine, these observations may be translated into practical proceedings to maximize the efficacy of LA by DSA. When conducting LA by DSA in HoFH patients, a filtration volume >4,000 mL should be targeted. Otherwise, LA by HELP remains more effective. Additionally, these data underscore the importance of lifestyle interventions (weight management and dietary counseling) in HoFH patients with hypertriglyceridemia.
In this study, the number of LA treatments using DSA in patients with double receptor-defective mutations was very limited. Although the analyses were adjusted for the LDLR genotype, it remains unclear whether the efficacy of LA with DSA was inversely associated with TG levels in subjects with double receptor-defective mutations. Hypertriglyceridemia is not a typical phenotypic characteristic of HoFH but it is well recognized that VLDL apoB-100 secretion is inversely associated with LDLR functionality.23, 24 The average fasting TG levels in patients with receptor-negative mutations were higher than those with receptor-defective mutations. The inverse association between pre-treatment TG concentrations and the efficacy of LA by DSA is particularly relevant for patients with double receptor-negative mutations. Therefore, the data from this study underscores the fact that these patients should be treated more intensively than patients with receptor-defective HoFH, as previously suggested.