Formation le génotype du récepteur LDL, tutoriel & guide de travaux pratiques en pdf.
Research letter
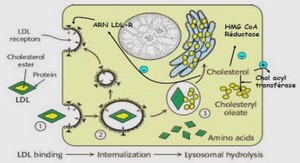
In homozygous familial hypercholesterolemia (HoFH) caused by mutations in the LDL receptor (LDLR) gene, patients with two receptor-negative mutations have higher cholesterol concentrations and coronary heart disease (CHD) risk than patients with double receptor-defective mutations.1
Pharmacological treatment is insufficient to achieve an efficient reduction in LDL-cholesterol (C) or lipoprotein (a) (Lp(a)) concentrations in HoFH patients, and repetitive long-term lipoprotein apheresis (LA) remains the gold-standard therapy. LA induces an acute decrease in LDL-C and Lp(a) concentrations, which is then followed by a rebound in the following days. The post-LA rebound constitutes a major determinant of LA efficacy as it directly affects the average concentrations between treatments, considered the best estimate of the physiological effects of long-term LA.2 However, our understanding of the determinants of post-treatment rebound in LDL-C and Lp(a) is very limited.2
This study aimed to determine the extent to which the LDLR genotype modulates the post-LA rebound in LDL-C and Lp(a) concentrations among HoFH patients. We hypothesized that the rebound in LDL-C and Lp(a) concentrations is greater among receptor-negative HoFH patients than among receptor-defective HoFH patients.
Data on all consecutive LA treatments performed between August 2008 and February 2016 among HoFH patients with genetically-defined defective/defective LDLR mutations (n=3), negative/negative LDLR mutations (n=8) and defective/negative LDLR mutations (n=4), treated at the CHU de Québec-Université Laval were collected. For each patient, the compiled data included: 1) date of LA, 2) cumulative number of LA treatments received, 3) interval between LA treatments, 4) LA system used,
5) volume of filtered plasma per treatment, 6) duration of treatments, 7) pre- and post-LA lipoprotein concentrations and 8) the cumulative interval since the first compiled LA treatment. Data on LDL-C and Lp(a) rebound covered 1999 and 1567 treatments, respectively. The rebound was calculated as the percentage difference between post-LA and pre-LA concentrations of the subsequent LA treatment. Mixed models for repeated measures with patients as a random effect were used for statistics. The study was approved by the Laval University Medical Center ethical review committee, and informed consent was obtained from each patient.
At baseline, patients (34.2 ± 14.3 years; women, n=8/15; CHD history, n=8/15) were treated with maximally tolerated dose of statin (atorvastatin: 80 mg, n=7; 40 mg, n=1; rosuvastatin: 40 mg, n=6; 5 mg, n=1) and ezetimibe and had cutaneous and tendinous xanthomas. Patients were French-Canadians (n=13), Lebanese (n=1) and Hondurian (n=1).
The LDLR genotype was significantly associated with LDL-C rebound (P=0.003). Negative/negative patients had a greater mean rebound in LDL-C concentrations compared with defective/defective patients and defective/negative patients, independent of the interval since the last treatment and drug therapy (Figure, A). Similar observations were obtained when the analysis was conducted with the rebound in absolute LDL-C levels in mmol/L. No interaction was observed between the LDLR genotype and the interval between treatments for the rebound in LDL-C (P genotype*interval =0.06). Therefore, differences in the rebound in LDL-C levels between LDLR genotypes were maintained over time. Moreover, weekly treatments were associated with significantly lower rebound in LDL-C levels compared with treatments conducted at longer intervals, independent of the LDLR genotype and drug therapy (Figure, B).
No difference was found in the rebound in Lp(a) concentrations according to the LDLR genotype. Nonetheless, the rebound in Lp(a) associated with weekly treatment was significantly lower than the rebound associated with bi-monthly treatments (117 ± 37% vs 166 ± 36%, P=0.0002).
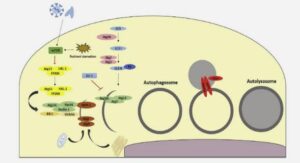
This retrospective longitudinal study demonstrates that the LDLR genotype is a significant determinant of the rebound in LDL-C concentration following LA among HoFH patients. It was estimated that the receptor-negative HoFH patients treated every 3 to 5 days would exhibit a rebound in LDL-C concentrations similar to one of the receptor-defective HoFH patients treated at an interval of 7 to 14 days. Mechanisms underlying the greater rebound in LDL-C observed in receptor-negative patients than in receptor-defective patients remain unclear, but are likely to rely on the impact of LDLR deficiency on apoB metabolism. Indeed, several studies have reported a direct inverse association between LDLR functionality and apoB secretion.3 In addition, it is likely that the efficacy of statins to inhibit cholesterol synthesis, which differs between receptor-negative and receptor-defective patients, could modulate post-LA LDL-C rebound.4, 5 Nevertheless, receptor-negative HoFH patients may benefit from more frequent LA to reduce their exposure to apoB-containing lipoproteins.
The number of treatments and the ~8 year follow-up are major strengths of the present study. However, these observations are reported from a limited number of mutations in the LDLR gene highly prevalent among the French-Canadians. A similar assessment among patients carrying other common LDLR mutations is warranted.
This study demonstrated that the rebound in LDL-C levels was markedly greater among receptor-negative than among receptor-defective HoFH patients. In order to optimize long-term benefits of LA in an era of precision medicine, this study underscores the importance of the screening for the LDLR mutation, the relevance of adapting LA therapy to the severity of the disease and the benefits associated with more frequent treatments.
Acknowledgments
Drs Couture and Lamarche designed the study. J.-P. Drouin-Chartier collected the data. J.-P. Drouin-Chartier and Drs Lamarche, and Couture analyzed the data. J.-P. Drouin-Chartier and Drs Tremblay, Bergeron, Lamarche, and Couture wrote the article. Dr Couture has full access to all the data and takes responsibility for its integrity and the data analysis.
Sources of funding
J.-P. Drouin-Chartier is a recipient of doctoral scholarships from the Fonds de recherche du Québec
– Santé and the Canadian Institute of Health Research.
Disclosures
Dr Couture has received funding in the last 5 years from the Canadian Institutes for Health Research, Agriculture and Agri-Food Canada (Growing Forward program supported by the Dairy Farmers of Canada (DFC), Canola Council of Canada, Flax Council of Canada, Dow Agrosciences), Dairy Research Institute, Dairy Australia, Danone Institute, Merck, Pfizer, Atrium Innovations and the Kaneka Corporation. Dr Lamarche is the Chair of Nutrition at Laval University, which is supported by private endowments from Pfizer, La Banque Royale du Canada and Provigo-Loblaws. BL has received funding in the last 5 years from the Canadian Institutes for Health Research, the Natural Sciences and Engineering Research Council of Canada and Merck. The other authors report that they have no conflicts of interest.